Treatment of allergic eosinophilic asthma through engineered IL-5-anchored chimeric antigen receptor T cells
Over 339 million people suffer from asthma worldwide, and patients with severe eosinophilic asthma (SEA) are at high risk of mortality and low quality of life. SEA is a significant phenotype of refractory asthma with poor clinical control. Biomarkers targeting the interleukin-5/IL-5 receptor α axis show promising therapeutic effects for SEA patients. Chimeric antigen receptor (CAR) is a fusion protein composed of an extracellular target-specific scFv-moiety and an intracellular T-cell receptor domain, typically CD28 and CD3ζ. Recently, adoptive immunotherapies based on CD19-specific CAR-T cells have shown remarkable efficacy in treating B cell malignancies.
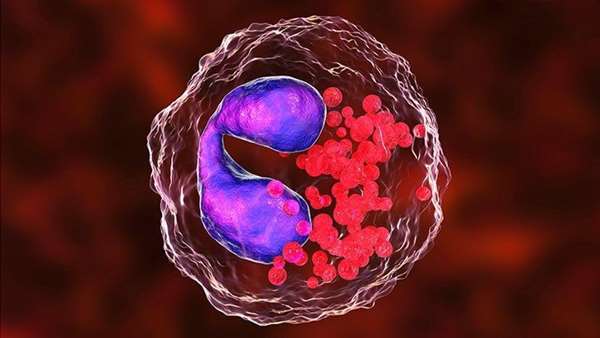
When engineered into primary T-cells, IL-5-anchored CCAR-T Cells( cytokine-anchored chimeric antigen receptor) specifically target eosinophils and progenitor cells. Researchers engineered eosinophil-targeting hIL-5Rα-specific T cells using two different CAR configurations. The first design follows the conventional CAR blueprint, comprising an extracellular scFv-moiety derived from benralizumab fused to an intracellular TCR-derived CD28-CD3ζ signaling domain. The second design uses the human IL-5 as the CAR extratermolar domain instead of scfv. Both CAR-T variants, generated through retroviral transduction of murine primary T cells, showed cytotoxicity against stable hCCR3-target cells in vitro.
Next, they tested the function of hIL-5-anchored CCAR-T cells in mice through bioluminescence imaging and intraperitoneal injection into NCG mice. They found that both murine primary and human primary CCAR T cells dramatically reduced eosinophil levels in response to exposure to UTD-T cell (un-transduced T-cells) therapy. The mIL-5 (IL-5-anchored CCAR retrovirus) has been implicated in developing asthma and allergic eosinophilic inflammation in mice.
MIL-5 is a type 2 cytokine that promotes differentiation and activation of eosinophils and is an essential biomarker for asthma. They found that IL-5-anchored CCAR-T cells led to a significant decrease in the level of inflammatory cells in the bronchial epithelium (BALF) following exposure to aerosols. These findings suggest that the concept might set a new standard for long-term protection against airway inflammation. Eosinophilic inflammation plays a prominent role in asthma, but current treatments can only control the symptoms to a certain extent. Scientists developed cellular adoptive immunotherapy using design principles adopted from chimeric antigen receptor-T cells and applied them to allergic asthma. To avoid anaphylaxis reactions typically observed in scFv-dependent CAR-T therapies, they employed a ligand-anchored CAR design that allows cytokines to trigger target-specific T-cell killing.
منبع:
Chen, S., Chen, G., Xu, F. et al. Treatment of allergic eosinophilic asthma through engineered IL-5-anchored chimeric antigen receptor T cells. Cell Discov 8, 80 (2022). https://doi.org/10.1038/s41421-022-00433-y



ارسال به دوستان