The human liver has amazing regeneration capabilities: Even if up to 70 percent of it is removed, the remaining tissue can regrow a full-sized liver within months.
Taking advantage of this regenerative capability could give doctors many more options for treating chronic liver disease. MIT engineers have now taken a step toward that goal, by creating a new liver tissue model that allows them to trace the steps involved in liver regeneration more precisely than has been possible before.The new study has identified one molecule that appears to play a key role.
Most of the patients who need liver transplants suffer from chronic illnesses such as viral hepatitis, fatty liver disease, or cancer. However, if researchers had a reliable way to stimulate the liver to regenerate on its own, some transplants could be avoided.From studies in mice, researchers have learned a great deal about some of the regeneration pathways that are activated after liver injury or illness. One key factor is the reciprocal relationship between hepatocytes and endothelial cells, which line the blood vessels. Hepatocytes produce factors that help blood vessels develop, and endothelial cells generate growth factors that help hepatocytes proliferate.
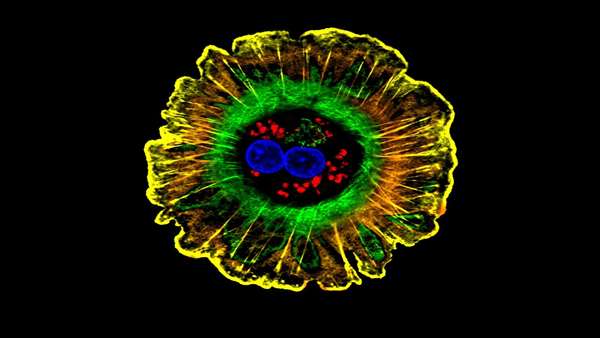
Another contributor that researchers have identified is fluid flow in the blood vessels. In mice, an increase in blood flow can stimulate the endothelial cells to produce signals that promote regeneration.To create these models of “regeneration on a chip,” the researchers grew blood vessels along one of these microfluidic channels and then added multicellular spheroid aggregates derived from liver cells from human organ donors.
The chip is designed so that molecules such as growth factors can flow between the blood vessels and the liver spheroids.Using this system, the researchers showed that increased fluid flow on its own did not stimulate hepatocytes to enter the cell division cycle. However, if they also delivered an inflammatory signal (the cytokine IL-1-beta), hepatocytes did enter the cell cycle.
By knocking out the gene for PGE2 biosynthesis in endothelial cells, the researchers were able to show that those cells are the source of PGE2, and they also demonstrated that this molecule stimulates human liver cells to enter the cell cycl.
In this study, the researchers focused on molecules that stimulate cells to enter cell division, but they now hope to follow the process further along and identify molecules needed to complete the cell cycle.
https://news.mit.edu/2022/liver-tissue-regeneration-model-0627



ارسال به دوستان