Tiny bubbles and a bit of gene therapy heal major bone fractures in pigs
It takes more than a cast and a little time to heal many broken bones. Whether it’s a soldier wounded in battle, a car accident victim, or an elderly person who has fallen, bone damage can be so extensive that the bones never heal properly, leaving people crippled or with other severe problems. Now, researchers have combined ultrasound, stem cells, and gene therapy to stimulate robust bone repair
It takes more than a cast and a little time to heal many broken bones. Whether it’s a soldier wounded in battle, a car accident victim, or an elderly person who has fallen, bone damage can be so extensive that the bones never heal properly, leaving people crippled or with other severe problems. Now, researchers have combined ultrasound, stem cells, and gene therapy to stimulate robust bone repair. So far the work has only been performed in animals. But it has already been so successful that it’s expected to move quickly toward human clinical trials.
The new research “has huge clinical significance,” says David Kulber, who directs the Center for Plastic and Reconstructive Surgery at Cedars-Sinai Medical Center in Los Angeles, California, and who was not part of the study. “The technology of being able to stimulate bone growth is really remarkable.”
It’s also one for which there is a glaring need. In the United States alone, some 100,000 people a year suffer from what is known as a nonunion fracture. In these cases, parts of a bone may be missing altogether or so badly splintered that the bone can’t be reassembled. In such cases, doctors typically graft other bone into the site. Ideally this bone comes from the same person—often taken from the pelvis, a painful procedure that compounds a person’s injuries and recovery time. When this isn’t possible, physicians will turn to cadavers for the extra bone. But this bone must be sterilized before it’s implanted, robbing it of proteins and other signaling molecules that encourage its regrowth once transplanted, and lessening the chances of a full recovery.
Researchers have long tried to improve matters by growing new bone without use of a graft. To do so they typically first fill gaps in bone with a natural scaffolding material called collagen. This scaffolding encourages a person’s own bone-forming stem cells, called mesenchymal stem cells (MSCs), to migrate into the area. The trouble is MSCs don’t only differentiate into osteocytes, the bone-producing cells. They can also develop into either fat tissue cells or scar tissue.
Researchers have tried for years to steer MSCs into becoming osteocytes by exposing them to one or more bone morphogenetic proteins (BMPs), signaling molecules that trigger the cells to transform into bone-forming cells. But for this differentiation to occur, MSCs must be exposed to BMPs for up to a week. Yet if the BMPs are simply injected into the site of a fracture, they dissipate in just hours.
In an effort to produce a lasting BMP signal, researchers led by Dan Gazit, a regenerative medicine expert at Cedars-Sinai, as well as other groups, have previously turned to using viruses to introduce extra copies of BMP genes into MSCs so that the cells themselves will produce the proteins long enough to trigger their own differentiation. But success has been halting here, too.
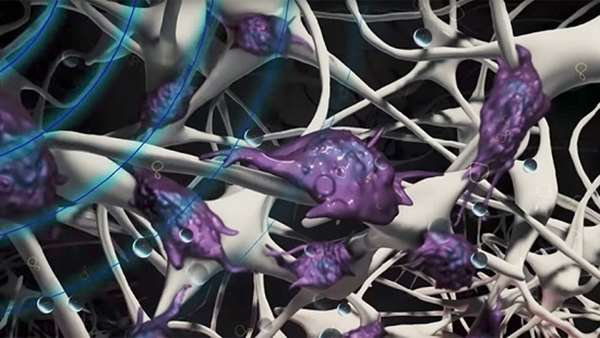
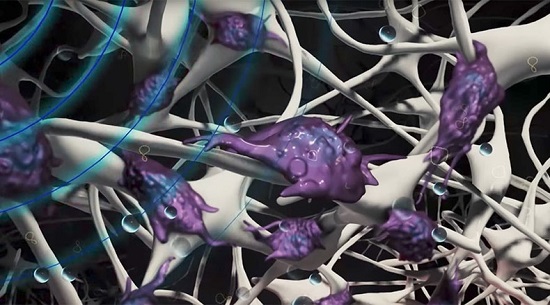
Over the last several years, Gazit’s team—among others—has developed an alternative strategy for efficiently getting genes into MSCs without viruses. The researchers start by packing the wound with the usual collagen matrix and waiting for a couple of weeks for the stem cells to infiltrate the scaffold. They then create a solution containing numerous copies of their gene of interest alongside gas-filled micron-sized bubbles encased by a thin shell of fat molecules. After injecting this solution into the fracture site, they go over the area with an ultrasound wand, much as it’s done by obstetricians to check on the health of a fetus. The wand’s ultrasound pulses burst the microbubbles, briefly punching nano-sized holes in any adjacent stem cells, which allows the genes in the solution to enter.
In 2014, Gazit and his colleagues reported that they used this procedure to introduce nontherapeutic reporter genes into large fractures in animal models. But when they used the procedure to introduce genes for two different BMPs—BMP-2 and BMP-7—they detected some bone regrowth in the animals, but not enough to heal the fractures.
Gazit’s group has gotten better results by using the same approach to insert copies of the gene for BMP-6 into pigs that had been surgically given 1-centimeter gaps in a leg bone. After waiting 8 weeks, they found that the bone gap was closed and the leg fracture was healed in all of the treated animals. In fact, the procedure was so effective that the fractures healed as well as when bone grafts were carried out using bone from the same animal, the currently preferred treatment, they report today in Science Translational Medicine.
The results are “just the type of thing we need to move this field forward,” says Johnny Huard, an orthopedics researcher at the University of Texas Health Science Center in Houston. However, he notes, the pigs used in this study were all under 1 year in age. Younger animals, including people, tend to have far more MSCs than older ones, he says, yet large fractures are far more common in the elderly than the young. So Huard suggests that before the approach is ready for testing in people with bone fractures, it would be good to first see whether it’s equally successful in older animals.
Reference: https://www.ncbi.nlm.nih.gov/pubmed/28515335



ارسال به دوستان