Stem-cell based therapy for type 2 diabetes and obesity
An article published in Experimental Biology and Medicine details a new therapeutic strategy for obesity and type 2 diabetes. The study, led by Dr. Bing Wang, Professor in the Department of General Surgery at Shanghai Ninth Peoples Hospital and Shanghai Jiao Tong University School of Medicine in Shanghai, China, reports that transplantation of adipose tissue-derived mesenchymal stem cells improves metabolic balance and reduces inflammation in an animal model.
An article published in Experimental Biology and Medicine details a new therapeutic strategy for obesity and type 2 diabetes. The study, led by Dr. Bing Wang, Professor in the Department of General Surgery at Shanghai Ninth People"s Hospital and Shanghai Jiao Tong University School of Medicine in Shanghai, China, reports that transplantation of adipose tissue-derived mesenchymal stem cells improves metabolic balance and reduces inflammation in an animal model.
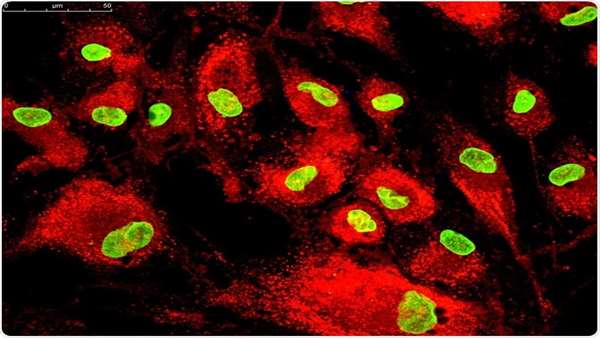
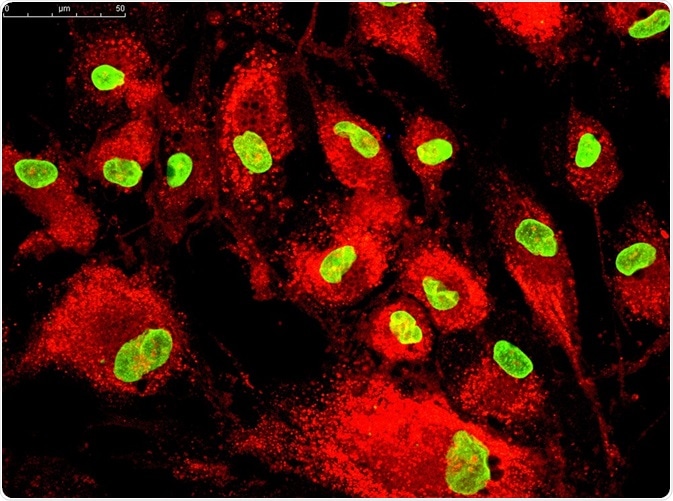
Sedentary lifestyles, along with high-fat and high-sugar diets, have made diabetes a global epidemic. The World Health Organization estimates that 90 percent of the 347 million people worldwide with diabetes have type 2 diabetes (T2D). In T2D, the body does not use insulin correctly, a process called insulin resistance. Initially, the pancreas makes extra insulin, but over time it cannot make enough insulin and blood glucose levels rise. If not treated, high blood glucose levels damage the heart, kidney, nerves and eyes. Obesity is a contributing factor for T2D diabetes, and the inflammation that occurs in obesity exacerbates insulin resistance. A preliminary clinical study has shown that transplantation of mesenchymal stem cells improves metabolic balance in patients with T2D. Adipose tissue-derived mesenchymal stem cells (ADSCs) are abundant and can be harvested with minimally invasive procedures. However, their ability to improve metabolic function in T2D or obesity is not known.
In the current study, Dr. Wang and colleagues assessed the ability of ADSCs to ameliorate insulin resistance in a high-fat diet (HFD)-fed mice. HFD-fed mice receiving ADSCs exhibited reduced blood glucose levels and enhanced insulin sensitivity. More importantly, ADSCs overexpressing neuregulin 4, a growth factor with beneficial effects in obesity and T2D, were the most effective in reducing blood glucose and insulin resistance. Finally, these protective effects were due to the suppression of inflammation and augmentation of glucose uptake in skeletal muscle and adipose tissues. Collectively, these studies demonstrate that ADSC transplantation improves glucose tolerance and metabolic balance in HFD-fed mice by multiple mechanisms. Dr. Wang, senior author for the study, said, "Our study shows that neuregulin overexpression could improve the efficacy of ADSCs in ameliorating insulin resistance and other obesity-related metabolic disorders and may provide a new therapeutic strategy for the treatment of obesity, insulinresistance and T2D."
Dr. Steven R. Goodman, editor-in-chief of Experimental Biology & Medicine, said, "Wang and colleagues have provided a potential new therapeutic option for type 2 diabetics who are obese. The use of adipose-derived mesenchymal stem cells and increased levels of neuregulin 4 led to reduced blood glucose and insulin resistancein mice fed a high-fat diet. If future clinical trials using this approach are efficacious, this will provide a valuable new treatment for type 2 diabetics."
Reference:https://journals.sagepub.com/doi/10.1177/1535370219839643



ارسال به دوستان