Self-assembled particle gel for promoting blood vessel formation
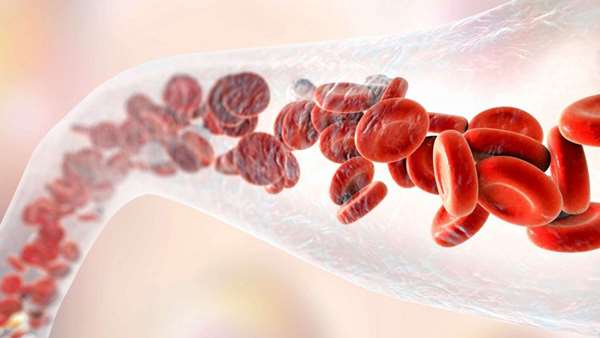
NIMS has developed a low-cost self-assembled particle-based injectable gel for promoting blood vessel formation—a regenerative medicine process vital in cell and tissue transplantation.
NIMS has developed a low-cost self-assembled particle-based injectable gel for promoting blood vessel formation—a regenerative medicine process vital in cell and tissue transplantation. This material may be used as an effective, low cost regenerative medicine technology and may serve as an alternative to expensive and deactivation-prone growth factors.
Current approaches to regenerating damaged biological tissues comprise transplantation of cells (i.e., injection of a cell suspension) and engineered tissues formed from cells cultured in test tubes. Because damaged tissues cannot form sufficient blood vessels to supply oxygen and nutrients to transplanted cells and tissues, these transplants fail to establish at target sites in patients' bodies. The use of growth factors for promoting blood vessel formation has been researched, but these growth factors are expensive and their effectiveness tends to degrade with time. For this reason, the development of new techniques that can promote blood vessel formation without using growth factors has been anticipated.
This research group focused on lipopolysaccharides (LPSs) with an ability to induce mild inflammation in human bodies, thereby triggering macrophages to produce growth factors. Inspired by the fact that an LPS molecule bears an alkyl group 12 to 14 carbons in length, the research group added 12-carbon alkyl groups to Alaska pollock-derived gelatin, thereby transforming it into spherical particles. Saline was then added to the particles, allowing alkyl groups to interact hydrophobically and forming a self-assembled gel. Injection of this gel into mice was found to cause microphages to produce growth factors, which in turn promoted the formation of new blood vessels. The injected gel degrades naturally in the body after new blood vessels are formed.
Simple injection of this material into patients' bodies can promote the formation of blood vessel networks. Using this technique, vascular beds may be formed at target sites in patients' bodies before cultured cells and tissues are transplanted to the locations, thereby effectively facilitating the recovery of biological functions. In addition, the use of this material is expected to reduce medical costs by eliminating the need for expensive growth factors prone to deactivation. In future studies, the research group plans to pursue the use of this new material in regenerative medicine and medical devices through collaborative medicine-engineering research
Reference:https://www.nature.com/articles/s41427-020-0229-4



ارسال به دوستان