Ovarian cancer: Scientists find a way to launch dual attack
Antibody therapy is a type of immune therapy, or immunotherapy, that uses enhanced antibodies to identify disease targets and then kill them or summon immune cells to kill them.
Antibody therapy is a type of immune therapy, or immunotherapy, that uses enhanced antibodies to identify disease targets and then kill them or summon immune cells to kill them.
Its success in treating ovarian cancer and other solid tumors, however, has been somewhat limited.
A reason for this is the hostile microenvironment of the tumor, which makes it hard for antibodies designed to kill cancer cells to reach them.
Now, scientists at the University of Virginia School of Medicine in Charlottesville have developed an approach that looks set to overcome this barrier.
They describe their "single-agent dual-specificity targeting" method for ovarian cancer in a study paper that features in the journal Cancer Cell.
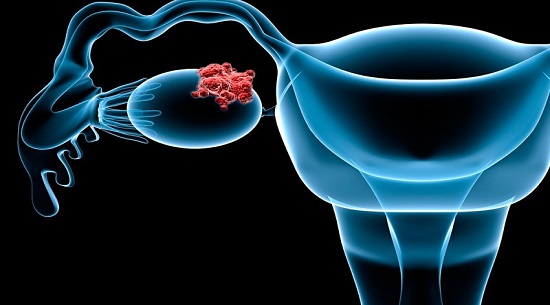
The approach uses a "two-pronged" antibody that hits two targets on the ovarian cancer cell.
One target is a protein called folate receptor alpha-1 (FOLR1), which is highly expressed in ovarian cancer. The antibody uses this target to home in on the cancer cell and "anchor" itself to it. The other target is another protein called death receptor 5. By binding to this protein, the antibody activates cell death.
"There are a lot of efforts," says study senior author Jogender Tushir-Singh, who is an assistant professor in biochemistry and molecular genetics, "in terms of cancer immune therapy, but the success of these are really limited in solid tumors."
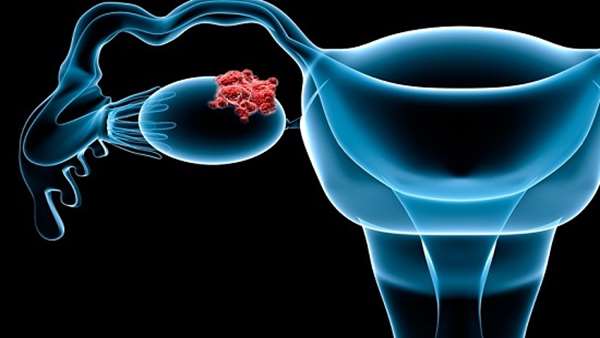
In the United States, ovarian cancer is the fifth most common cause of cancer deaths in women. Of all the cancers that affect women"s reproductive system, it is the deadliest.
The American Cancer Society (ACS) estimate that "about 22,240 women" will find out that they have ovarian cancer in 2018, and around 14,070 will die of the disease.
Antibody therapies are immunotherapies that use engineered antibodiesthat are highly skilled at finding and attaching themselves to specific substances on cancer cells. For this reason, they are also called "targeted therapies."
Some of these therapies use the antibodies as markers so that other immune cells can more easily spot their targets and destroy the cancer cells.
Others — such as the type that Tushir-Singh and team decided to work on — use antibodies that can also stop the cells dividing or even kill them. There is also another type that uses the antibodies to ferry drugs to the tumor cells.
Ovarian cancer forms solid tumors, meaning that the malignant growths do not usually contain liquid or cysts. Other examples of this cancer type include breast cancer and prostate cancer.
Solid tumors pose a big challenge to antibody therapies because they have microenvironments whose conditions, such as low oxygen, make it difficult for immune cells to survive and do their work.
Tushir-Singh explains that another challenging feature of the solid tumor microenvironment that occurs in ovarian cancer in particular is that "some unusually large receptors form a protective fence around tumor cells, so even if the immune cells reach there, there are many obstacles."
So, he and his colleagues focused on how to overcome the hostility of the microenvironment. This is how they came up with the idea of antibodies with "two heads."
One head attaches to the cancer cell"s FOLR1 protein, while the other head focuses on killing it by triggering the death receptor. FOLR1 is already "well established" as a marker for ovarian cancers likely to have poor outcomes.
From laboratory tests that they did on cells and in mice, the scientists believe that the engineered antibodies are 100 times more powerful at killing ovarian cancer cells than those that have been tested in clinical trials.
Tushir-Singh says that another advantage of their approach is that it does not appear to produce the toxic side effects seen with many other antibody therapies.
What is often seen in antibody therapy is that a lot of the antibodies leave the blood too quickly and collect in the liver, causing liver toxicity. However, because their approach ensures that the antibodies find a "good home" in the tumor, they are kept "away from the liver," Tushir-Singh explains.
The researchers eventually want to test the method in human trials, although there is still a way to go before it is ready for that. They need to find funding for further preclinical testing and to file an investigational drug.
Tushir-Singh suggests that — with some modifications — the approach might also be used to treat other solid tumors, such as those of breast and prostate cancer.
In addition, it might also be possible to use it to "revive" some antibody therapies that have shown disappointing results.
Reference:https://www.cell.com/cancer-cell/fulltext/S1535-6108(18)30310-6



ارسال به دوستان