Clinical researchers at Hannover Medical School (MHH) have succeeded for the first time in stopping the usually fatal course of pulmonary hypertension thanks to a novel therapeutic approach. A three-year-old girl suffering from so-called pulmonary arterial hypertension (PAH) was treated a total of five times with mesenchymal stem cell products obtained from a human umbilical cord.
"The treatment led to a significant improvement in growth, exercise tolerance and clinical cardiovascular variables and reduced the number of plasma markers in the blood that can be detected in vascular constriction and inflammation," says Professor Dr. Georg Hansmann, head of the Translational Cardiopulmonary Biomedicine research group, and lead attending physician in the Department of Paediatric Cardiology and Intensive Care Medicine. After six months, not only was there a clear improvement in health, but there were also no undesirable side effects.
This is the first time there is a therapy for people suffering from pronounced forms of pulmonary hypertension. "Further studies are needed to confirm and explore the benefits of this new stem cell therapy," Professor Hansmann emphasizes. The research was published in Nature Cardiovascular Research.
PAH is a disease in which the blood pressure in the pulmonary circulation is chronically elevated—hence the name pulmonary hypertension. The cause of the high pressure is usually narrowed lung vessels and/or a loss of these vessels. The disease is progressive and usually fatal. In advanced stages, PAH is considered non-curable. The currently approved PAH drugs are mainly aimed at vasodilatation.
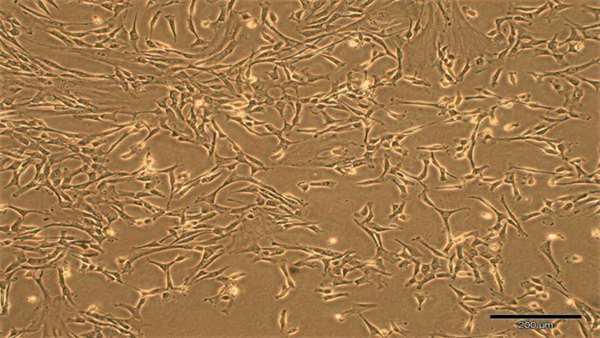
Repetitive mesenchymal stem cell therapy is based on cells from the umbilical cord of newborns and is also called HUCMSC (human umbilical cord mesenchymal stem cell). The researchers' analyses showed that the products of these stem cells from the umbilical cord were able to improve regeneration in the damaged blood vessels, inhibit inflammation of the blood vessels and curb damage to certain parts of the cells.
"We have evidence that this HUCMSC-derived therapy had multiple beneficial effects: in the heart of the treated patients, it mainly protected the energy-providing mitochondria, and in the lungs the treatment mainly inhibited inflammation and stimulated regeneration," explains Professor Hansmann, "We can show that the proteins, lipids and prostaglandin E2 are enriched in the stem cells and its products, and that MSC-derived therapy modulate several key signaling pathways of PAH at once."



ارسال به دوستان