CRISPR/Cas9 Disrupts Glaucoma Gene, Takes Pressure off Eyes in Disease Models
Scientists at the University of Iowa could be forgiven if they were to revise an old nursery rhyme to read, “two blind mice.” The scientists, led by Val Sheffield, M.D., Ph.D., used the CRISPR/Cas9 gene-editing system to disrupt a gene known to cause glaucoma.
Scientists at the University of Iowa could be forgiven if they were to revise an old nursery rhyme to read, “two blind mice.” The scientists, led by Val Sheffield, M.D., Ph.D., used the CRISPR/Cas9 gene-editing system to disrupt a gene known to cause glaucoma. Then the scientists determined that in a mouse model of glaucoma, disruption of the gene prevented high intraocular pressure, an early precursor to the most common form of glaucoma, which is known as primary open-angle glaucoma (POAG).
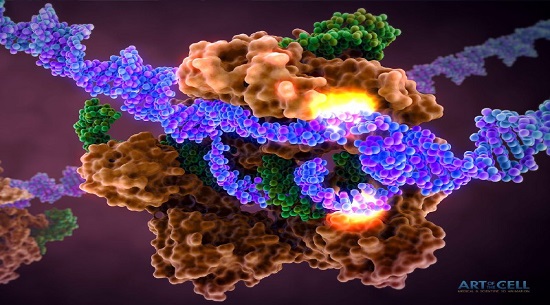
Dr. Sheffield and colleagues used CRISPR/Cas9 to prevent expression of a mutated version of the myocilin gene, or MYOC. This intervention not only prevented glaucoma in the mouse model, it also eliminated myocilin expression in culture human cells, as well as in ex vivo human eyeballs. Taken together, these results raise hopes that CRISPR/Cas9-based treatments could be used to prevent myocilin-associated glaucoma.
"As scientists, we dont want to just discover a ‘diseased gene,’ we want to understand what the gene does and, in this case, have a better understanding of glaucoma so that it can be more effectively treated," said Dr. Sheffield. "No one knows what this gene does, except that its mutant form causes glaucoma."
Glaucoma is a common vision and neurodegenerative disorder affecting 3% to 5% of people over the age of 40. It often begins with POAG, which itself is presaged by high intraocular pressure—fluid pressure inside the eye—that damages retinal ganglion axons at the optic nerve and leads to death of retinal ganglion cells that carry the visual signals to the brain, which can cause blindness.
Myocilin is a protein found in the trabecular meshwork, a part of the eye that regulates intraocular pressure. When the myocilin gene is mutated, it can produce a variant form of the myocilin protein, which can then cause high intraocular pressure. Mutations in myocilin are implicated in juvenile- and adult-onset primary open-angle glaucoma.
A means of disrupting the sequence of events that lead to glaucoma was evaluated in a study led by Dr. Sheffield. The results of this study appeared October 2 in the Proceedings of the National Academy of Sciences, in an article entitled “CRISPR-Cas9–Based Treatment of Myocilin-Associated Glaucoma.” This article described how Dr. Sheffield’s team used in vitro human trabecular meshwork cells, an in vivo mouse model, and ex vivo human eyes to assess the potential of clustered regularly interspaced short palindromic repeats (CRISPR)-mediated genome editing in human myocilin-associated POAG.
“By disrupting the mutant myocilin gene and its function using CRISPR-Cas9, we were able to reduce associated endoplasmic reticulum stress, lower intraocular pressure, and prevent further glaucomatous damage in mouse eyes,” the study’s authors wrote. “We also show the feasibility of using the CRISPR-Cas9 system in cultured human eyes.




ارسال به دوستان