Boy with Hemophilia A Undergoes Successful Stem Cell Transplant
A number of clinical studies have reported that bone marrow-derived cells contribute to the production of clotting factor VIII (FVIII), the molecule linked to hemophilia A.
A number of clinical studies have reported that bone marrow-derived cells contribute to the production of clotting factor VIII (FVIII), the molecule linked to hemophilia A. Because the current treatment for this bleeding disorder is associated with some disadvantages and risk, hematopoietic stem cell transplant (HSCT) has become an emerging therapy approach for these patients.
In this study, researchers describe the case of a 4-year-old boy with mild congenital hemophilia A who underwent a successful HSCT.
The research paper, “Successful Allogenic Haematopoietic Stem Cell Transplantation in a Boy with Hemophilia A and MDS-RAEB,” was published in Klinische Padiatrie.
Treatments to manage hemophilia A, a disease caused by a deficiency of FVIII, has led to an increase in patients’ life expectancy. But risks exist, including developing leukemia or other neoplasia later in life, along with elevated incidences of diseases like HIV and hepatitis C.
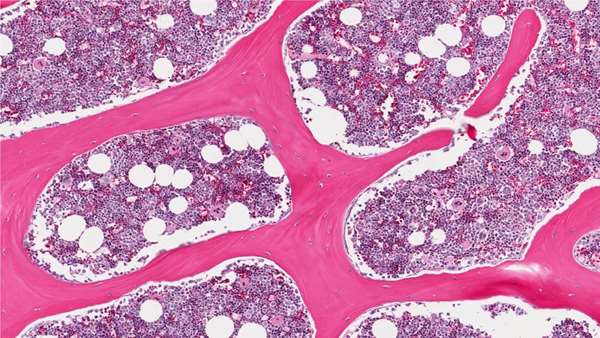
This may indicate that more patients with hemophilia A and other bleeding disorders may need HSCT. While the liver is the main production site of FVIII, some studies have also reported a contribution of bone-marrow derived cells to FVIII-
production, but little is known about the clinical relevance of this fact.
In this study, researchers said the boy who underwent allogeneic (from a donor) HSCT was first assessed at age 2, when he presented with easy bruising, prolonged partial thromboplastin time (PTT) — a test used to assess how long the blood takes to clot — and marked thrombocytopenia, the clinical term for platelet deficiency.
However, due to an unremarkable bone marrow analysis and a recent upper airway infection, the symptoms were attributed to another condition and ultimately resolved.
At age 4, the boy presented again with increasing bleeding symptoms and prolonged PTT and he was eventually diagnosed with mild hemophilia A with a residual FVIII-activity of 18 percent in absence of FVIII-inhibitors. Additional examinations revealed MDS-RAEB (myelodysplastic syndrome-refractory anemia with excess blasts). MDS is considered a type of cancer and occurs when the blood-forming cells in the bone marrow are damaged, which leads to low levels of any type of blood cell.
After HSCT, the FVIII activity spontaneously increased to a maximal level of 45 percent, remained elevated for four weeks, but ultimately declined to pre-HSCT levels two months later. The child’s recovery to the procedure went well, with no associated toxicity or immune system rejection.
“At the last follow-up the patient was well and in stable hematological remission. F-VIII-activity was 19.6 percent and he did not present any bleeding symptoms,” the researchers wrote.
Despite limited resource studies evaluating HSCT for hemophilia A, the researchers concluded that the procedure is not clinically relevant in terms of FVIII production.
“Although the experience is very limited, current clinical studies do not provide evidence for a relevant contribution of donor bone marrow-derived progenitors to FVIII-synthesis,” they wrote.



ارسال به دوستان