Blood stem cells produced in vast quantities in the lab
Researchers have managed to grow large numbers of blood-forming stem cells in the lab using a surprisingly simple ingredient found in glue. And when injected into mice, the cells started producing key components of blood.
Researchers have managed to grow large numbers of blood-forming stem cells in the lab using a surprisingly simple ingredient found in glue. And when injected into mice, the cells started producing key components of blood.
“The finding is very unexpected and exciting,” says John Dick, a stem-cell biologist at the Prince Margaret Cancer Centre in Toronto, Canada.
If the technique can be applied to humans, it could be used to grow blood stem cells for use in people with blood cancers such as leukaemia whose immune systems have been damaged by chemotherapy. The approach could also provide a safer way to treat people with blood disorders, such as sickle-cell disease, who currently have to undergo a risky procedure before receiving a bone-marrow transplant.
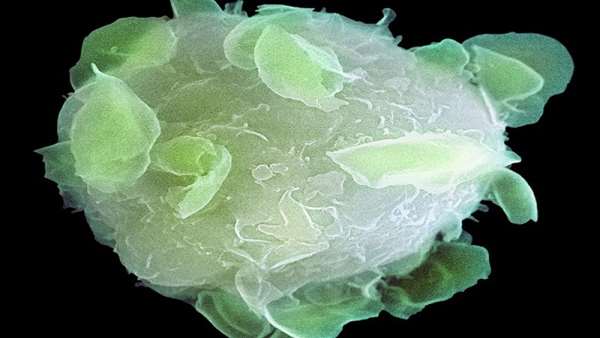
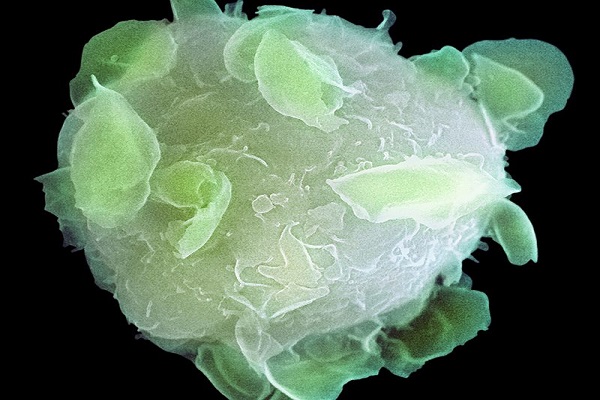
Researchers have been trying for decades to grow in the lab large numbers of ‘haematopoietic’ blood stem cells (HSCs), which regenerate themselves and give rise to other blood components. But until now, none had been able to produce the number needed to reliably engraft — or start producing blood cells — when reintroduced into the body.
Stem-cell biologist Hiromitsu Nakauchi, who leads teams at the University of Tokyo and Stanford University in California, reports in Nature on 29 May how his team managed to successfully engraft HSCs in mice1. The researchers first expanded a cluster of mouse HSCs to almost 900 times its original level in just a month, then transplanted them back into a different set of mice, where they thrived and developed into blood components. “This has been my life goal,” he says.
Usually, an animal’s immune system will try to destroy donor cells that aren’t a genetic match. That is why immune systems have to be eliminated or suppressed before most transplants. But when Nakauchi injected the cells into healthy mice with intact immune systems, the cells thrived, possibly, he says, because of the large numbers introduced. Nakauchi is now working on adapting the technique to grow human HSCs.
The study offers the best evidence yet that lab-grown HSCs can survive for more than a few days and engraft when reinserted into the body, says George Daley, a stem-cell biologist at Harvard School of Medicine in Boston, Massachusetts, who also has worked on expanding HSCs. “These are impressive data,” he says.
“This level of expansion could have a huge impact in the clinic,” says Paul Frenette, a haematologist at Albert Einstein College of Medicine in New York City.
Magic material
Researchers looking for ways to grow HSCs in large numbers in the lab had tried using growth factors without much success. But Nakauchi found that the reason the cells weren’t surviving was impurities in the medium in which the cells were being grown, a human blood protein called albumin. These impurities, mostly proteins released by immune cells, were stopping the cells from growing, says Nakauchi. “How much money, time, and effort has been wasted because of those impurities!” he says.
Nakauchi screened a bunch of polymers that he thought could replace albumin, and found that a synthetic compound called polyvinyl alcohol (PVA), often used in glues, did the trick. PVA has also been used to culture embryos and embryonic stem cells. “It’s quite easy. People can go to Safeway and get glue,” Nakauchi says. Laboratory versions of PVA work better than those from the supermarket, he says, and the polymer, which is used in tablet coatings, is deemed non-toxic by regulatory agencies.
Connie Eaves, a stem-cell and cancer researcher at the Terry Fox Laboratory in Vancouver, Canada, and others are keen to try the technique. But Eaves warns that it is still unclear whether it will work with human cells.
Nakauchi’s findings could renew attention on another source of HSCs. In 2017, Daley reprogrammed human skin cells into induced pluripotent stem (iPS) cells that then developed into cells that were very close to blood stem cells2. The advantage of using iPS cells to make HSCs over obtaining them through a bone marrow transplant from a donor is that they can be made from a patient’s own cells, removing the need for a genetically matched donor. But Daley has struggled to grow large numbers of these cells in the lab. Nakauchi"s method could change that. “If this method is applicable to human cells, it could be very helpful,” he says.
Avoid ‘conditioning’
Nakauchi’s team also demonstrated that mice could receive the donor HSCs without first undergoing a process to destroy or suppress their immune system, known as conditioning.
People with genetic blood disorders such as sickle-cell disease are sometimes treated with a bone-marrow transplant from a donor. Since donors, even siblings, are not a genetic match, the patient first has to undergo conditioning to stop their body from rejecting the donor cells. But the conditioning increases the risk that the donor HSCs will attack the host’s tissues, a potentially fatal disease. It can also make people infertile and impede growth in children.
The idea of reducing the need for conditioning by transplanting a ‘mega-dose’ of HSCs is attractive, but requires further testing, first in mice and then in humans, says Luigi Naldini, who researches gene therapy using HSCs at the San Raffaele Hospital in Milan, Italy.
And if Nakauchi’s technique works with human cells, researchers could also extract HSCs from patients and use gene-editing tools to correct any disease-causing mutations, before reintroducing the cells into the patients. Because the cells would be from the patient rather than a non-matched donor, conditioning would not be necessary, says Nakauchi.
Reference:https://www.nature.com/articles/d41586-019-01690-w



ارسال به دوستان