Developing a human neural organoid is like building an airplane while it hurtles down the runway. Yes, that’s a cliché, but it’s apt. Among other things, it explains why human neural organoids still lack a consistent nomenclature—let alone engaging user manuals.
“We shouldn’t use [the term] mini-brains; it’s inaccurate and demeaning,” notes Sergiu P. Paşca, MD, professor of psychiatry and behavioral sciences at Stanford University and director of the Stanford Brain Organogenesis Program. “Humanized animals” should also be avoided, he adds, “because we’re not humanizing the cells.”
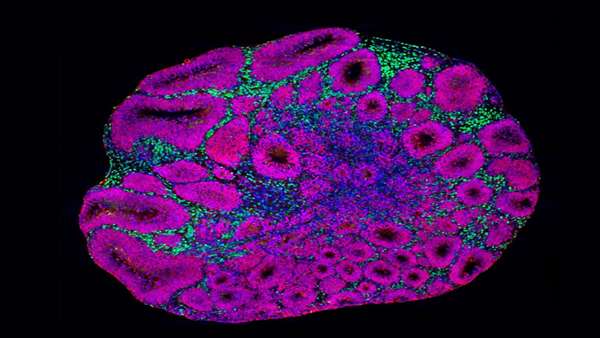
Although an accurate and dignified name has yet to be agreed upon, scientists can offer established descriptions. For example, organoids can be described as self-organizing, 3D, cellular models, typically derived from human pluripotent stem cells. Bennett G. Novitch, PhD, professor of neurobiology, University of California, Los Angeles (UCLA), says that neural organoids incorporate different cells that are ordinarily found in the human brain, and that organize, under laboratory conditions, in a manner that approximates many features of the real human brain.
Formal, systematic efforts to establish a consistent nomenclature include a recent perspective article in Nature.1 In this article, a small group of organoid researchers provides a framework for the nomenclature of “human multicellular models of nervous system development and disease, including organoids, assembloids, and transplants.” They deprecate the terms mini-brain, brain-in-a-dish, and whole-brain. In contrast, they approve of the terms neural organoids and nervous system organoids. In addition, since nervous system organoids are from specific brain regions, an additional suggestion is to coin region-specific terms such as cortical organoids, retinal organoids, hypothalamic organoids, and spinal cord organoids.
Neural organoids have evolved from objects of hype to systems that are solid enough to support useful studies. Although improvements continue to be made, notes Paola Arlotta, PhD, chair of the Harvard Department of Stem Cell and Regenerative Biology, currently available neural organoids are already being used to study mechanisms of disease or principles of brain development that could not be studied otherwis Developing neural organoids, then, is a little like building a plane that is already in flight. Neural organoids, like many technological wonders, started with “a lot of hype—probably at the time when it was too early,” Arlotta says. But she adds that the excitement was justified: “You could see through it—you could see that the research was going to start a new field and a new way of thinking.”
Sound roots and robust growth
The organoid field has come a long way in a short amount of time, moving through several phases since its inception, Novitch observes. The first phase was spent proving that organoids could be made. The second phase, which is currently underway, focuses on establishing phenotypic models of disease. The third phase, which is already starting, is about using the disease-modeling organoids to delineate disease pathways and advance drug development.
Although the field started over a decade ago, the most dramatic advances occurred fairly recently. According to Novitch, the momentum has picked up over the past five to six years. He adds that while there are still challenges and a tendency to indulge in hype, the technology is on the verge of being able to do many things. He is convinced that when it comes to understanding fundamental mechanisms of human brain development and disease, neural organoids are poised to make very big advances over the next few years. Novitch adds that some of the research going on today—for example, using organoids as avenues into neurogenetics—is approaching a real connection to human patients
Not all organoids are alike
Organoid experiments, Novitch cautions, are not for the faint of heart. That said, when he is reviewing grants, he sees more and more researchers “throwing in an organoid aim.” Although he appreciates the interest in the platform, Novitch worries that overly enthusiastic researchers could overlook potential problems.
Novitch calls the field the “Wild West,” largely due to issues with consistency. There are many different protocols for making organoids. In addition, different laboratories have different time frames. So, a “week 5” organoid may not be the same from one laboratory to another. This can be particularly challenging when comparing transcriptomic studies. He says that when there is dissimilarity in the developmental progression or the cell types in an organoid, misunderstandings can get “really ugly.”
Novitch drives this point home in a recently published paper.2 The findings in the paper show that when cells of the same type are grown by different methods, markedly different outcomes are possible—even when the same organoid protocol is used. Arlotta agrees that reproducibility has been a problem in the field. Although she does not think that the problem is completely solved, she notes that the field has “gone a long way to address this.”
Novitch proposes that the field needs a set of established guidelines for quality control—a reference to compare populations of cells between laboratories. Without guidelines, the alignment of findings is very challenging.
Arlotta agrees and thinks that this topic is bound to garner a lot of attention in the near future. She says that the sheer number of protocols ensures that there is no such thing as one human brain organoid. And although the organoid field is still relatively small, it is “expanding like crazy,” she notes. As the field grows, so too does the need to make sure that all researchers are speaking the same language when they make claims about reproducibility, cell types, and disease modeling.
The development of good organoid practices is a work in progress, Novitch remarks. Currently, he is collaborating on a review article that tackles the subject and attempts to harmonize the many opinions held by scientists at the UCLA Intellectual and Developmental Disabilities Research Center (IDDRC). (The UCLA IDDRC, where Novitch co-directs the Cells, Circuits, and Systems Analysis Core, is one of 14 IDDRCs supported by the National Institute of Child Health and Human Development.)
To make matters more complicated, commercial kits meant to simplify organoid experiments are proliferating. Arlotta says that the kits are exactly why the field needs standards. Once the standards are established, it almost doesn’t matter where the protocol comes from, as long as there is clarity and transparency about what you get in the end.
Mapping organoids
Arlotta’s laboratory recently published an article presenting a “single-cell transcriptomic, epigenetic, and spatial atlas of human cortical organoid development.”3 The atlas, she says, reflects an effort to “dig really deep” into organoids. It is also, in the words of
the article’s authors, meant to “prime investigation into the mechanisms of human cortical development.”
In this article, Arlotta and colleagues describe how they traced the entire developmental trajectory in single-cell multiomics space, as well as how they built a lineage tree of the cells of the human brain for the first time in vitro. The authors also suggest that their lineage tree could facilitate the study of human-specific mechanisms for the differentiation of brain cells. Such mechanisms are usually considered difficult or impossible to study because human brain cells develop mostly in utero.
Let the genetics play out
In organoids, the study of structural phenotypes, like the study of circuitry, seems intuitive. But many researchers, including Paşca and Arlotta, are interested in using organoids to study neuropsychiatric disorders. In neuropsychiatric illness or a neurodevelopmental disease such as autism, it’s different—there is nothing that appears obviously wrong when you simply look at the brain of a patient with schizophrenia. But Arlotta argues that organoids are useful in this space because there is a lot of genetic information associated with the risk of some of these diseases.
Using that genomic information, researchers can grow an organoid that models the genome of a person. This provides a way to design experiments in an unbiased, adventurous way. Arlotta’s team took this approach to study autism in work published earlier this year in Nature.4 The team grew organoids from different donors in order to explore the roles of three different autism risk genes (SUV420H1, ARID1B, or CHD8).
“We had no idea what we were going to find,” she says. But the organoids were a hypothesis generator, the likes of which the researchers never had before. Now, for the first time, studies can let the genetic information play out, and let it make a primitive brain—with circuits and things that you can watch and study and phenotype.
Organoids offer a unique understanding of what the genomes of patients do. We can leverage genetic information, says Arlotta, to understand what is going on and find cellular targets and molecules. This is a huge opportunity that did not exist in animal models, simply because they did not address the need for the human genome.
Clearing hurdles
Organoids typically lack sensory input. This is a limitation of the system because it misses the role that brain activity plays in brain development and maturation. Arlotta thinks that “incorporation of activity, in a process of development of the organoid, will be critical for the next step.”
Paşca’s group has been working on that next step for about seven years. At the end of October, his group published a paper in Nature5 showing how human neural organoids matured in the brains of newborn rats. Although organoids have been transplanted into adult rat brains for years, the younger brains yielded different results. When the human neural organoids were transplanted into the somatosensory cortex of the newborns, they grew (becoming six times larger than when grown in vitro), partially integrated into neural circuits, and demonstrated functionality. In addition, links were established between the organoids’ activity and animal behavior. And when the rats’ whiskers were touched, the organoids responded to the stimulation.
The next step for Paşca is to transplant assembloids, or groups of organoids, with different ratios of excitatory and inhibitory neurons. The interactions of these cells in the cortex are key to understanding diseases like epilepsy.
Paşca and colleagues believe that using this system will allow them to ask questions that cannot be asked using other models. This system has already helped the scientists begin testing drugs for neurodevelopmental and neurodegenerative diseases.
The key thing to remember, Novitch stresses, is that organoids are human cells. Because of that, organoids give researchers the opportunity to model diseases more faithfully than they could with other systems. And that alone gives the researchers a huge advantage over many of the other methods that have been used in the past.
https://www.genengnews.com/topics/translational-medicine/neural-organoids-making-connections-getting-real/



ارسال به دوستان