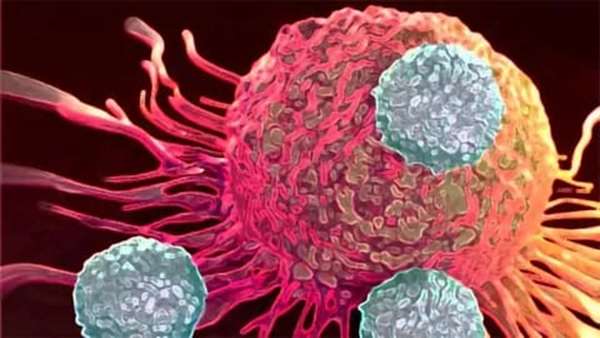
T-cell therapy is a growing field, with applications moving beyond treating blood cancers to treating solid tumors too. Progress is also being made towards using T-cell therapy to treat infectious diseases such as human immunodeficiency virus (HIV) and influenza.
One of the conventional types of T-cell therapy relies on the development of a chimeric antigen receptor (CAR) to target diseased or cancerous cells specifically, but a subset of T cells, called gamma-delta (γδ) T cells, could enable cell-specific targeting without the need for the CAR. The γδ T cells act as a bridge between the innate and adaptive immune systems, and as such work as an effective immunotherapeutic by recruiting immune responders, such as natural killer (NK) cells to a tumor.
Technology Networksspoke to Bryan Kobel, the CEO of TC Biopharm about the broad uses of γδ T-cell therapy and how they approached developing Omnimune, a pioneering treatment for acute myeloid leukemia (AML) that has shown promise in a Phase IIb/III clinical trial.
Katie Brighton (KB): Can you discuss the impact that T-cell therapy is having across different disease areas?
Bryan Kobel (BK): Right now, we’re seeing a real wave of cell therapies being pushed into the clinic across a number of diseases. Central nervous system diseases, infectious diseases and diabetes, to name a few. Largely, these therapeutics are still to be pushed out to the public, but I think the biggest impact to date has been a shift in how we perceive patient treatment. It has become more of a focus to find treatments that work in harmony with our existing system, versus previously, where the focus was more about inventing something completely foreign to the body to treat a disease state. As more of these cell therapies are used in the clinic – and we see more data – inherently we will learn and understand more about not just the therapeutic, but hopefully about how the body is affected by the disease in question and how we can further enhance therapeutic options for patients. Cell therapies also seem to have low toxicity profiles, so the future of this field is opened further to potential collaborations and combination therapies in difficult diseases.
KB: What makes γδ T cells advantageous for T-cell therapy, compared to other T-cell subsets?
BK: There are a number of advantages to the γδ T cell; it’s quite a unique cell. The receptor on the γδ T cell is composed of gamma and delta chains, enabling it to bridge between the innate and adaptive immune systems. Therefore, its function isn’t as isolated as that of other T-cell subsets. Specifically, the mechanism of action of the γδ T cell is dependent on the presence of a phosphoantigen by the name of isopentenyl pyrophosphate (IPP). IPP is expressed by sick and diseased cells (including all tumors ever studied) and is not expressed by healthy cells. As such, the γδ T cell is targeted toward tumor cells without having to be modified. As part of its immune system function, γδ T cells orchestrate the immune response. If γδ T cells are targeting a site of infection or a tumor, they will bring other immune responders like NK cells with them. This makes the γδ T cells not only the first responders to diseased tissues such as fungal infections and cancer cells, but also a signal to the immune system that it needs to kick the defense mechanisms into high gear.
KB: What diseases can or are being targeted by γδ T-cell therapy?
BK: There are several companies in the γδ T-cell therapy space doing interesting things – right now the majority of γδ therapy work is being conducted in oncology settings. Currently, there are ongoing trials or recent data for non-Hodgkin’s lymphoma, glioblastoma, AML and a number of other solid tumor efforts. Companies like In8bio, Adicet, Lava Therapeutics and Imcheck Therapeutics are all working in the γδ therapy
space in varying ways and we are seeing more and more positive data from the sector. The current uses of γδ T-cell therapy in oncology look promising, although there is still a good amount to learn.
Beyond oncology, there is strong evidence that γδ T cells can be a well-tolerated and efficacious therapeutic in infectious or viral disease states. We’ve seen some evidence in trials of fungal and bacterial infections being
addressed by the γδ T cells and we know part of their function is to target diseased cells before the virus or infections can spread. The majority of this work is preclinical or anecdotal, but there’s certainly a strong scientific premise and rationale for using γδ T cells for diseases such as severe influenza, fungal infections in the gut and for viruses including HIV and Ebola.
KB: TC BioPharm has just commenced a Phase IIb/III clinical trial with its OmnImmune product for AML. Can you talk to us about how OmnImmune was developed and how it works for treating AML?
BK: OmnImmune was the natural progression of our platform after running an autologous trial in solid tumors. When TC BioPharm was originally formed, the cofounders Angela Scott and Dr. Mike Leek made the conscious decision to focus on γδ T cells and also to build our manufacturing capabilities in-house so we would be vertically integrated. As we went through the original autologous trial, we learned quickly that the process of treating sick patients with their own γδ T cells would be uneconomical and potentially not as efficacious due to immune suppression, cell exhaustion and a number of
other issues (for example, the product not being able to be “off-the-shelf” in nature). With that data, the obvious next step was to leverage our core expertise and advance to allogeneic T-cell work, the product now dubbed OmnImmune. We knew the γδ T cells had an antitumor effect from our original trial, it was now about getting the best possible therapeutic to the patient.
Since γδ T cells are not major histocompatibility complex-restricted, they’re naturally a perfect allogeneic therapeutic, with no graft-versus-host disease and also no toxicity that we’ve seen. OmnImmune was the progression of the platform to where the γδ T cells can be most powerful, as an allogeneic off-the-shelf cancer treatment.
The γδ T-cell effect on AML in our Phase 1b trial was pretty stellar. Despite the trial being cut short, we saw strong responses, with stable disease in one patient at our low dose 28 days after treatment and 2 complete responses (including one morphologic leukemia-free state) for the medium dose 28 days post-injection. Unfortunately, our next patients were cut short, one due
to disease progression and one due to COVID-19, although we did get safety data and saw efficacy signals at 14 days post-injection in the patient whose therapeutic intervention had to be cut short due to COVID-19. The reason this is exciting is around the aforementioned premise of the universal mechanism of action. Since the γδ T cells react to IPP, which all tumors express, we were of the mindset that we can help reinforce your immune system with its natural fighters in the form of γδ T cells and let them do their jobs as nature intended.
So, the question is really, “Can we get enough of the γδ T cells into the patient’s system to fight against the disease and do it safely?” I think we answered that emphatically on both ends, meaning OmnImmune can be used at multiple points of the treatment paradigm, the γδ T cells will provide an efficacious therapeutic effect against AML and we can provide this at a price point that’s extremely economical compared to today’s treatments.
Additionally, and looking farther out, since IPP is present in all blood cancers it stands to reason we might see efficacy using unmodified γδ T cells in other
hematological cancers like acute lymphocytic leukemia, chronic lymphocytic leukemia, multiple myeloma and others.
KB: What challenges exist when working to develop safer, efficacious and cost-effective cell therapy products?
BK: There are probably too many to recount here! Cell therapy is still in the early stages, maybe not in its infancy but certainly not fully matured. We are still learning about the actions of the cells, the subvariants, still advancing manufacturing technology and on and on.
I think the clear and present challenges today surround the move to allogeneic cell therapy. Creating a safe and efficacious product using universal donor banks or donor cells is a very tall task. We’re lucky to have a great development team with Dr. Emilio Cosimo and Daria Paruzina working every day to advance our capabilities in that arena, including moving OmnImmune to a frozen/thawed product which they accomplished during the
coronavirus pandemic. We also have our secret weapon in Angela Scott, who’s been in cell therapy good manufacturing practice for decades, bringing a wealth of knowledge on how to advance our products safely into the allogeneic aren
Being cost-effective really means you need to get to a point where you can deliver the product on a campaign manufacturing basis and deliver it at the point of care. As a result, you need economy of scale and that includes when we move towards modified products or in the combination arena. It’s not an easy problem to solve, but I’m confident in our team at TC BioPharm and also the brilliant people in the cell therapy industry at large to solve these issues and put cell therapy at the forefront of the therapeutic arena.
KB: What are TC BioPharm’s next steps for advancing treatments for cancer and infectious diseases?
BK: Our next steps really hinge around gaining clinical data for OmnImmune in blood cancers and our modified
CAR γδ approach in solid tumors. OmnImmune is potentially an extremely versatile therapeutic that can be used at multiple points of treatment for patients with AML and also could potentially show efficacy in other blood cancers, given the universal mechanism of action around IPP. Additionally, the therapeutic being low to nonexistent on the toxicity profile makes it an ideal candidate for combination therapies, so we could look at something like a combination therapy for late-stage patients with dwindling options. You could envision this as almost a maintenance therapy.
For solid tumors, our development team is working diligently to complete our proof-of-concept work and preclinical work using a CAR T approach with γδs. This could potentially be a paradigm shift in CAR programs, using the γδ T cells’ response to IPP (or lack thereof in the absence of IPP) as an on/off switch to avoid onsite or off-tumor toxicity. Dr. Emilio Cosimo’s team developed a biological circuit of sorts around dual activation signals to activate the kill signal for the CAR γδ T cells, so both the CAR T-cell receptor and the cell receptor on the γδ T cells both need to attach and send an activation signal. If the CAR attaches to a healthy cell, it will send activation signal number one, but if the γδ T cells does not sense the presence of IPP, it will not send activation signal number two, so the circuit is not completed and the cell-
killing power of the therapy is not unleashed, very similar to an electrical circuit not being completed. This could allow for the dosing levels to be high enough without toxicity to get the therapeutic out of the vasculature and into the tissue. Therefore, it’s an exciting time as we advance our oncology platform over the next 6–12 months.
On the infectious disease front, we are looking at a number of angles relating to treating oncology patients with suppressed, compromised or weakened immune systems including fungal infections likeAspergillusand other common infectious diseases such as influenza.
https://www.technologynetworks.com/biopharma/blog/a-new-approach-to-t-cell-therapy-364507



ارسال به دوستان