Scientists from the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA have developed a technique that will enable researchers to more efficiently isolate and identify rare T cells that are capable of targeting viruses, cancer and other diseases.
The approach could increase scientists’ understanding of how these critical immune cells respond to a wide range of illnesses and advance the development of T cell therapies. This includes immunotherapies that aim to boost the function and quantity of cancer or virus-targeting T cells and therapies intended to regulate the activity of T cells that are overactive in autoimmune diseases such as diabetes and multiple sclerosis.
The study, published today in Proceedings of the National Academy of Sciences, describes how the new method, called CLInt-Seq, combines and improves upon existing techniques to collect and genetically sequence rare T cells.
“T cells are critical for protecting the body against both infections and cancers,” said Pavlo Nesterenko, first author of the new paper and a graduate student in the lab of Dr. Owen Witte. “They're both the effectors and organizers of the body’s adaptive immune response, which means they can be used as therapeutics and studying their dynamics can shed light on overall immune activity.”
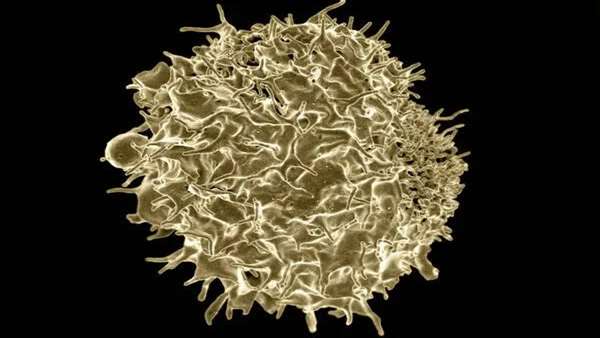
T cells stand out from other immune cells because they are equipped with molecules on their surfaces called T-cell receptors that recognize fragments of foreign proteins called antigens.
Our bodies produce millions and millions of T cells per day and each of these cells has its own distinct set of receptors. Every T-cell receptor is capable of recognizing one specific antigen. One T-cell receptor might recognize an antigen from the virus that causes the common cold while another might recognize an antigen from breast cancer, for example.
When a T cell encounters an antigen its receptor recognizes, it springs to action, producing large numbers of copies of itself and instructing other parts of the immune system to attack cells bearing that antigen.
Researchers around the world are exploring methods to collect T cells with receptors targeting cancer or other illnesses like the SARS-CoV-2 virus from patients, expand those cells in the lab and then return this larger population of targeted T cells to patients to boost their immune response.
“The problem is that in most populations of cells we have access to, whether it be from peripheral blood or samples taken from other parts of the human body, T cells with receptors of interest are found in very low numbers,” said Witte, senior author of the paper and founding director of the UCLA Broad Stem Cell Research Center. “Existing methods for capturing and identifying these T cells are labor-intensive and need improvement.”
Part of the reason this process is inefficient is that when T cells recognize the antigen for which they have the corresponding receptor, they send out signals that prompt other cells nearby to partially activate.
“These so-called bystander cells are excited by the activity around them, but are not really capable of reacting to the antigen that provoked the immune response,” said Witte, who holds the presidential chair in developmental immunology in the department of microbiology, immunology and molecular genetics and is a member of the UCLA Jonsson Comprehensive Cancer Center.
When researchers attempt to isolate T cells with specific receptors using traditional methods, they end up capturing many of these bystander cells. CLInt-Seq alleviates this problem by incorporating a technique that enables researchers to distinguish T cells with receptors of interest from most bystander cells.
Isolating T cells with specific receptors is only the first step. In order for these isolated cells to be useful, they need to be analyzed using droplet-based mRNA sequencing, also known as Drop-seq, which can measure messenger RNA expression in thousands of individual cells at once.
“Once you know the sequence of a T-cell receptor of interest, you can use that information to develop therapies that either make more of that cell in the case of fighting cancer and viruses or introduce regulatory T cells with this receptor sequence to curb an overactive immune response in a given area,” Nesterenko said.
The process of isolating T cells with specific receptors requires that the cells’ contents are fixed in place using chemicals that form bonds between the proteins inside each cell and their surroundings – this technique is known as cross-linking. Unfortunately, cross-linking degrades the T cells’ RNA, which makes Drop-seq analysis very challenging. CLInt-Seq overcomes this hurdle by utilizing a method of cross-linking that is reversible and thus preserves the T cells’ RNA.
“The innovation of this system is that it combines an improved method that identifies T-cell receptors with more specificity with a chemical adaptation that makes this process compatible with droplet-based mRNA sequencing,” Witte said. “This addresses challenges at the heart of finding T-cell receptors for treating cancer and other diseases as well as viral infections – from acute viruses like the virus that causes COVID-19 to chronic viruses like Epstein Barr or herpes.”
Moving forward, the Witte lab is utilizing this technology to address a number of scientific questions, including identifying T-cell receptors that react to the SARS-CoV-2 virus and developing T-cell therapies for prostate cancer.
This research was funded by the National Cancer Institute, the Parker Institute for Cancer Immunotherapy, a UCLA Tumor Immunology Training Grant and the UCLA Broad Stem Cell Research Center, including support from the Hal Gaba Director’s Fund for Cancer Stem Cell Research.



ارسال به دوستان