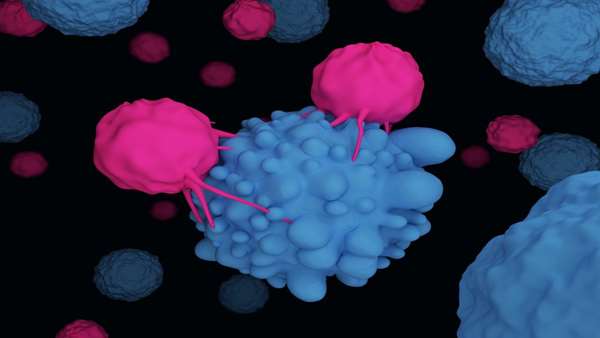
Relapse following chimeric antigen receptor (CAR) T-cell therapy directed against CD19 for relapsed/refractory B-acute lymphoblastic leukemia (r/r B-ALL) remains a significant challenge. Three main patterns of relapse predominate: CD19 positive (CD19pos) relapse, CD19 negative (CD19neg) relapse, and lineage switch (LS). Development and validation of risk factors that predict relapse phenotype could help define potential pre- or post-CAR T-cell infusion interventions aimed at decreasing relapse.
A group of scientists sought to extensively characterize pre-infusion risk factors associated with the development of each relapse pattern via a multicenter, retrospective review of children and young adults with r/r B-ALL treated with a murine-based CD19-CAR construct. Of 420 CAR-treated patients, 166 (39.5%) relapsed, including 83 (50%) CD19pos, 68 (41%) CD19neg, and 12 (7.2%) LS relapses. A greater cumulative number of prior complete remissions was associated with CD19pos relapses, whereas high pre-infusion disease burden, prior blinatumomab non-response, older age, and 4-1BB CAR construct were associated with CD19neg relapses.
The presence of a KMT2A rearrangement was the only pre-infusion risk factor associated with LS. The median overall survival following a post-CAR relapse was 11.9 months and was particularly dismal in patients experiencing a LS, with no long-term survivors following this pattern of relapse. Given the poor outcomes for those with post-CAR relapse, study of relapse prevention strategies, such as consolidative hematopoietic stem cell transplant, is critical and warrants further investigation on prospective clinical trials.



ارسال به دوستان