Spheroid co-culture of BMSCs with osteocytes yields ring-shaped bone-like tissue that enhances alveolar bone regeneration
Oral and maxillofacial bone defects severely impair appearance and function, and bioactive materials are urgently needed for bone regeneration. A critical-sized bone defect will not heal spontaneously and requires surgical reconstruction, so bone substitutes remain an urgent need. The main sources of bone transplantation for clinical use include autologous bone transplantation, allogenic or heterologous bone transplantation, and tissue-engineered construction. Autogenous bone grafts are widely regarded as the “gold standard,” but tissue availability and donor site morbidity limit this approach. Allografts and xenografts have clear limitations, including immunological rejection, infection risk, and lack of osteoinductive and angiogenic potential.
Therefore, tissue engineering has emerged as an attractive and alternative approach for bone regeneration. This method targets the generation of biological and living substitutes for damaged tissue to restore, maintain, or improve tissue function. Biomaterials for bone regeneration have been developed from inert materials that cannot interact with physiological tissue, but current iterations include bioactive materials that can stimulate osteoblasts. The biomaterials ideally should be able to promote osteogenic differentiation in vitro and bone formation in vivo.
Three-dimensional (3D) cell culture systems are increasingly used in the field because of its obvious advantages in providing more complex information about the physiology of the tissue. One promising 3D method is the spheroid culture system, which facilitates cell–extracellular matrix (ECM) and cell–cell interaction and provides a physiochemical environment similar to the in vivo experience. Spheroid-cultured cells are reported to have improved cell survival, stemness, multi-differentiation potential, as well as enhancing anti-inflammatory and angiogenic responses and bone formation in vivo.
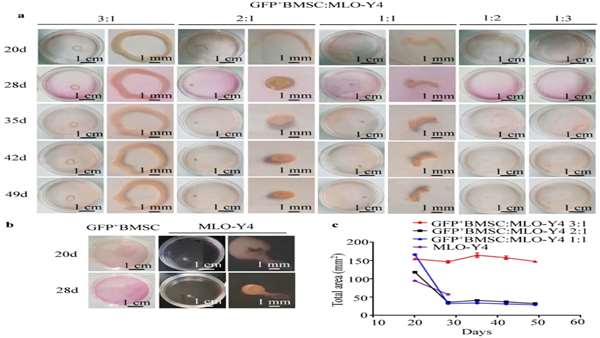
The selection of seed cells is important in bone regeneration. MSCs in bone marrow, umbilical cord blood, and adipose tissue have a considerable ability to regenerate bone tissue. Among these options, bone marrow stromal cells (BMSCs) have been suggested as an ideal seed cell source. the co-culture of BMSCs with osteocytes may promote osteogenic differentiation for bone regeneration. BMSCs can differentiate into the osteogenic lineage and form bone-like tissues both in vivo and in vitro and have been used in the clinical treatment of osteonecrosis, total joint arthroplasty, and cartilage defect repair.
Many cell types in bone tissue, including osteocytes, osteoblasts, and fibroblasts, can secrete ECM to form a natural and precisely arranged fibrous network that provides a specialized local microenvironment for tissue engineering. Among these options, osteocytes are the most abundant cell type in bone and the master orchestrators of bone physiology and homeostasis. osteocytes are more influential than osteoblasts in stimulating osteogenesis in BMSCs. the co-culture of BMSCs with osteocytes may promote osteogenic differentiation for bone regeneration.
In this study, bone-like tissue with an internal structure and mineral composition similar to mouse femur was formed via spheroid co-culturing of BMSCs and MLO-Y4 cells. The implantation of this tissue into tooth extraction sockets of mice demonstrated that it could promote bone formation and maturation, thus accelerating alveolar bone regeneration.
Researchers’ findings point to the potential for in vitro fabrication of bone-like tissue to mimic in vivo bone, opening the way to the development of new bioactive materials and treatment strategies for bone tissue engineering.
Zhou, YH., Guo, Y., Zhu, JY. et al. Spheroid co-culture of BMSCs with osteocytes yields ring-shaped bone-like tissue that enhances alveolar bone regeneration. Sci Rep 12, 14636 (2022). https://doi.org/10.1038/s41598-022-18675-x



ارسال به دوستان