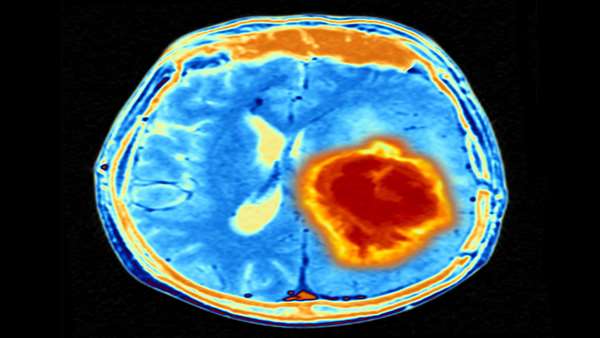
Glioblastomas (GBMs) are highly aggressive tumors of the brain and spinal cord that are challenging to treat because many cancer therapeutics cannot pass through the blood-brain barrier. Scientists headed by teams at Brigham and Women’s Hospital and Harvard Medical School have now devised a novel therapeutic strategy for post-surgical treatment of GBMs that uses biogel-encapsulated healthy donor-derived stem cells engineered to attack GBM-specific tumor cells. The results of a study, reported in Nature Communications, confirmed that the treatment was effective in preclinical models of GBM, with 100% of mice living for more than 90 days after treatment.
“This is the first study to our knowledge that identifies target receptors on tumor cells prior to initiating therapy, and using biodegradable, gel-encapsulated, ‘off-the-shelf’ engineered stem cell based therapy after GBM tumor surgery,” said Khalid Shah, PhD, director of the Center for Stem Cell and Translational Immunotherapy (CSTI) and the vice chair of research in the department of neurosurgery at the Brigham and Women’s Hospital, and faculty at Harvard Medical School and Harvard Stem Cell Institute (HSCI). “In the future, we will be applying this strategy to promptly identify target receptors after one receives a GBM diagnosis, then
administer a gel-encapsulated, off-the-shelf, engineered stem cell therapeutic from a pre-made reservoir.”
Shah and colleagues reported on the technology, and preclinical results, in a paper titled, “Target receptor identification and subsequent treatment of resected brain tumors with encapsulated and engineered allogeneic stem cells.” In their report, the authors concluded, “Upon validation, this study will pave the path to clinical testing in Phase I/II study in primary and recurrent GBM patient cohorts.”
While the last decades have seen advances in treatment strategies for different types of cancer, glioblastoma remains a major therapeutic challenge, the authors noted. Surgical resection followed by post-operative radio- and chemotherapies represent the current standard of care, but more than 90% of GBM tumors will return. And as the authors wrote, “ … patients generally succumb to the disease.”
Cell-based therapies offer a promising therapeutic strategy for these highly malignant brain tumors, but clinical translation is limited by what the team noted is “the lack of effective target identification and stringent testing in preclinical models that replicate standard treatment in GBM patients.”
Many cell-based therapies for cancer are derived from a patient’s own stem cells or immune cells. However, in a disease like GBM, most patients undergo surgery in the first
week after receiving their diagnosis due to the disease’s rapid progression, granting little time to develop therapeutics from their own cell types. “Considering the critical and very limited timeline from diagnosis to primary surgical intervention in GBM patients, allogeneic “off-the-shelf” engineered stem cells offer a promising therapeutic strategy to target residual GBM post-surgery,” the investigators pointed out. “Allogeneic cells can be fully characterized and banked, and therefore allow for the development of ‘off-the-shelf’ therapeutics for various clinical conditions, including brain tumors.”
The new cell therapy approach developed by Shah and colleagues cell therapy uses these allogenic stem cells—stem cells taken from healthy donor individuals—so that the treatment is readily available to administer immediately to patients at the time of surgery. For their study, the researchers evaluated the efficacy of several capsules that can carry the stem cell therapeutic in the brain, and generated a biodegradable hydrogel capsule that could successfully transport therapy without being cleared by the cerebrospinal fluid.
The team first identified specific receptors known as death receptors on circulating tumor cells (CTCs) in the bloodstream, using a genetic biomarker that is commonly expressed on tumor cells. “To identify CTC in blood circulation, we chose CD146 as a marker to select these rare CTC based on a positive screen of expression in our library of primary patient-derived GBM cells.”
The team then took stem cells (mesenchymal stem cells; MSCs) from the bone marrow of healthy human donors and engineered the cells to release a protein that binds to the death receptors and initiates cell death. They also built a herpes simplex virus-thymidine kinase (HSV-TK) safety switch, or “kill switch” into the stem cell system. When activated by ganciclovir (GCV) this kill switch effectively eradicates the stem cells. “Given that safety is paramount in clinical translation, it is essential to enhance the safety of the therapeutic,” they wrote. “Kill switches provide a unique way to safeguard therapeutics and add an additional layer of safety that can be controlled for biological therapies.”
The team assessed the efficacy of the therapeutic bifunctional mesenchymal stem cells (MSCBif) in animal models of primary and recurrent GBM tumors, post-surgery. Notably, all mice that received the gel-encapsulated stem cell-based therapeutic after surgery were still alive 90 days post-treatment. In contrast, mice that solely underwent surgery exhibited a mean survival time of 55 days. “We show that biodegradable hydrogel encapsulated MSCBif (EnMSCBif) has a profound therapeutic efficacy in mice bearing patient-derived invasive, primary, and recurrent GBM tumors following surgical resection.”
The investigators additionally assessed the safety of the treatment by conducting several studies using different doses of MSC therapy on mice. They found no signs of toxicity among mice with or without tumors. Imaging studies confirmed that triggering the kill switch did kill off the stem
cells, and also enhanced the anticancer effects. “Our PET imaging revealed that GCV-triggered HSV-TK kill switch successfully eliminated MSCBif after their administration into the tumor resection bed,” they noted. “We also observed that HSV-TK conversion of prodrug GCV further augmented GBM killing.”
It’s hoped that the study’s findings will pave the way to the start of Phase I clinical trial in patients with GBM undergoing brain surgery, within the next two years. “Our results confirm a highly efficacious therapeutic profile and a favorable toxicology evaluation, thereby presenting clinical promise for a first-in-human (FIH) study of EnMSCBif in GBM patients,” they suggested. “Studies outlined in this work were specifically performed to support an IND application, filed with the FDA to start an FIH study of these engineered MSC encapsulated in a biodegradable hydrogel to assess safety and tolerability in primary and recurrent GBM patients post-surgical debulking.”
Shah and colleagues noted that this therapeutic strategy will in addition be applicable to a wider range of solid tumors and that further investigations of its applications are warranted. “Beyond this therapy’s significant exhibited success rate, these findings suggest that we can use stem cells from healthy individuals to treat cancer patients,” said Shah. “This work lays down a foundation to begin building an engineered therapeutic stem cell biobank targeting different receptors on tumor cells and the immune cells in the tumor microenvironment that we will one day be able to use to treat
a wide range of difficult-to-treat cancers like GBM.”
The authors further concluded, “Following evaluation of the safety and tolerability in patients with recurrent and primary GBM in a Phase I trial, subsequent clinical trials might lead to robust use of allogenic MSC therapies for hard-to-treat cancers such as GBM.”



ارسال به دوستان