New CAR-T therapy shows promise against neuroblastoma
A novel CAR-T therapy has been developed by researchers at University College London (UK), with the purpose of targeting cancerous tumors. The investigators noted that the therapy has shown promising early results in children with neuroblastoma.
A novel CAR-T therapy has been developed by researchers at University College London (UK), with the purpose of targeting cancerous tumors. The investigators noted that the therapy has shown promising early results in children with neuroblastoma.
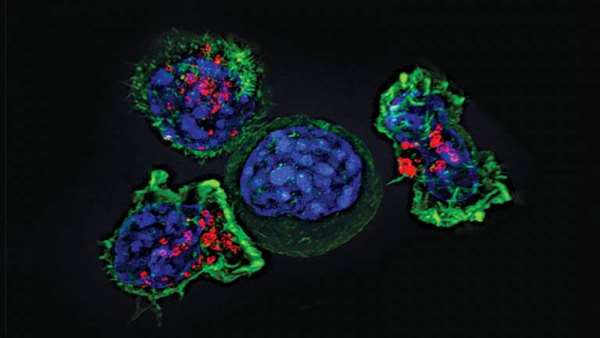
Within the study, the patients’ own T cells were modified with a CAR to target the GD2 surface protein, which is highly abundant on almost all neuroblastoma cells but is found in very low levels in healthy cells. When using a sufficient dose of the modified CAR-T cells, the researchers found that this treatment induced rapid reduction in tumor size in some of the patients treated.
For this proof-of-principle study, researchers at the UCL Great Ormond Street Institute for Child Health (GOS ICH) and the UCL Cancer Institute modified the patient’s own T-cells (a type of immune cell), equipping them to recognise and kill neuroblastoma tumour cells.
Twelve children with relapsed or refractory (where the disease does not respond to treatment) neuroblastoma were treated as part of the Cancer Research UK-funded phase I clinical trial.
Dr Sue Brook, medical advisor at Cancer Research UK, said: “Children who have hard to treat cancers like neuroblastoma have limited treatment options open to them, especially when the cancer returns.
“The early results for the GD2 CAR-T treatment look promising, especially due to the initial safety data. However more work is needed on making the response last longer, and we are looking forward to seeing the next steps in its development.”
The research team are preparing for their next clinical study in collaboration with Autolus, a clinical-stage biopharmaceutical company developing next-generation, programmed T-cell therapies for the treatment of cancer. This study will evaluate AUTO6NG, which builds on this approach utilising the same GD2 CAR alongside additional programming modules designed to enhance efficacy and persistence.
* To establish the minimal effective dose, escalating doses of GD2-directed CAR T-cells were used. The first group of patients was given a low dose, the second group a higher dose, and a third group a higher dose still. Each patient received one dose only. Researchers found that a minimal cell dose of 108/m2** was needed for the CAR T-cells to divide and become activated once administered to the patient.
** The dose is expressed per square metre surface area as this is a paediatric study and that is how doses are calculated in children (or alternatively per kilogram of body weight). The cell dose is 108 per square metre body surface area or 100 million cells per square metre body surface area.
https://www.regmednet.com/cell-therapy-weekly-new-car-t-therapy-shows-promise-against-neuroblastoma/



ارسال به دوستان