Mesenchymal Stem Cell Study Takes a Step Towards the Cell-free Treatment of Diabetes
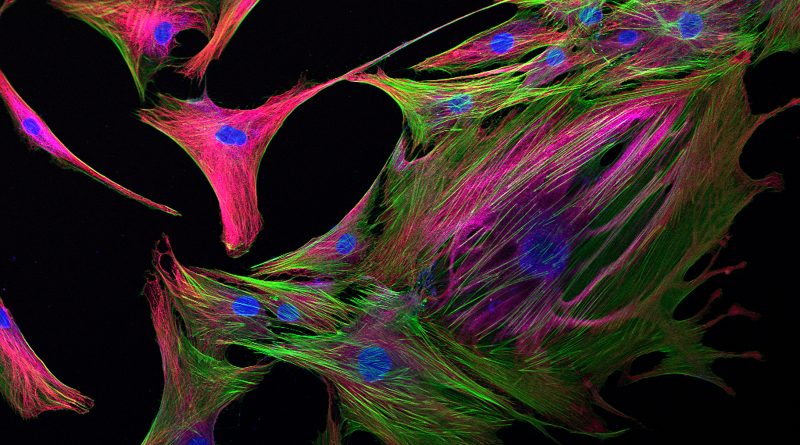
Previous studies on islet regeneration from the laboratories of Gilles A. Lajoie (Western University) and David A. Hess (Robarts Research Institute, London, Ontario, Canada) revealed that transplants of human bone marrow mesenchymal stem cells (hBM-MSCs) led to the emergence of small recipient‐derived islet‐like structures in the pancreas, thereby producing the β-cells required to battle the insulin deficiency associated with both type 1 and type 2 diabetes [1-3]
Previous studies on islet regeneration from the laboratories of Gilles A. Lajoie (Western University) and David A. Hess (Robarts Research Institute, London, Ontario, Canada) revealed that transplants of human bone marrow mesenchymal stem cells (hBM-MSCs) led to the emergence of small recipient‐derived islet‐like structures in the pancreas, thereby producing the β-cells required to battle the insulin deficiency associated with both type 1 and type 2 diabetes [1-3]. In search of mechanistic insights, subsequent proteomic analysis of secreted factors then highlighted Wnt‐signaling from hBM-MSCs as a central pathway mediated islet regeneration [4].
With this knowledge in hand, the duo now returns with a new STEM CELLS study that aimed to discover if secreted factors alone could regenerate the mouse islet by injecting hBM-MSC conditioned media into the mouse pancreas [5]. Kuljanin at al. now report on how the identification and validation of important hBM-MSC derived factors that promote islet regenerative may permit the development of cell‐free regenerative therapies for diabetic patients.
Initial analyses discovered that intrapancreatic‐injection of concentrated conditioned medium derived from hBM-MSCs stimulated islet regeneration in a dose-dependent manner without the need for cell transfer. Overall, the authors observed significantly reduced hyperglycemia, increased levels of circulating serum insulin, and improved glucose tolerance in a streptozotocin‐treated murine model of diabetes. Interestingly, the generation of conditioned medium in the presence of a glycogen synthase kinase 3‐inhibitor, which activates Wnt/β-catenin signaling, further accelerated and widened the observed β‐cell mass recovery.
By next studying the consequences of conditioned medium injection, the authors demonstrated that multiple regenerative factors promoted the emergence of proliferating insulin-positive cell clusters next to the ductal region. Cell emergence was then followed by the expression of the NKX6.1 β‐cell transcription factor in glucagon-positive cells, suggesting the conversion of pancreatic α‐cells into β‐cells, and then by accelerated β‐cell maturation with increased expression of the MAFA, a β‐cell transcription factor required for insulin production that marks mature, functional insulin‐secreting β‐cells. Of note, this regenerative process occurred over four days after a single administration of conditioned medium.
While these results support the development of cell-free regenerative therapies for diabetic patients, the authors note the requirement for preclinical testing in relevant models of autoimmune diabetes and the exploration of alternate modes of delivery before translating their findings to human patients. Of additional interest, the authors also highlight the additional role of hBM-MSC secreted factors in immunomodulation, an ability that may additionally dampen autoimmunity while boosting islet regeneration in type 1 diabetes patients.



ارسال به دوستان