A first-of-its-kind cancer treatment June and his team at the University of Pennsylvania were developing had shown striking early results in three patients in a small clinical trial. But funding had dried up and June couldn’t afford to treat anyone else.
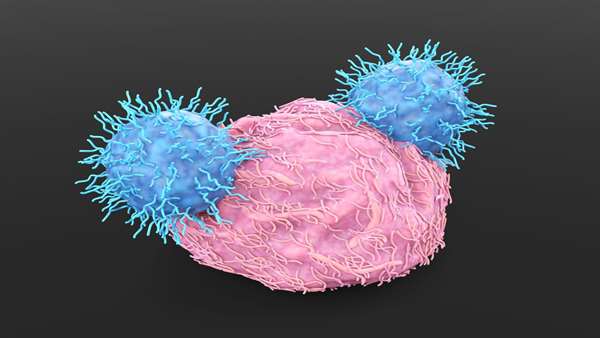
So June took a risk. He and his team wrote case reports on those first three patients, each of whom had received a cutting-edge treatment known as CAR-T cell therapy. They were sick with a form of leukemia that had evaded prior treatments, but all three went into remission after treatment — results so notable they were published in August 2011 in two major medical journals.
“It worked better than we ever thought it would,” said June, in an interview with BioPharma Dive. “That completely changed everything.”
June and his colleagues received thousands of requests from leukemia patients and even owners of sick pets to receive the treatment next. Offers from pharmaceutical companies and venture capitalists followed as the initial results were seen as a milestone in long-running efforts
to make cell therapies for cancer. June’s program was licensed to Novartis and became the drug now sold as Kymriah.
Other therapies developed in the biotechnology startups Kite Pharma and Juno Therapeutics also reached market, stamping CAR-T as a powerful and potentially curative treatment.
Since then, funding hasn’t been a problem for June, whose next act has been to found biotech startups. One, Tmunity Therapeutics, has raised at least $175 million since 2015. Another that debuted last month, Capstan Therapeutics, has already secured $165 million. Both are part of a wave of companies trying to prove cell therapy can work in solid tumors and in autoimmune diseases.
“There’s an emerging cell therapy industry,” June said. “It’s a very exciting time.”
Challenges remain. The Food and Drug Administration last year halted trials of Tmunity’s lead program for prostate cancer after two trial participants died. Capstan’s goal — to have the body make its own CAR-T cells with the help of messenger RNA — has never been attempted in humans. Other types of cell therapies
based on different cell types or using alternate production techniques have shown limitations, too.
BioPharma Dive spoke with June about his experience founding startups and the future of the field. The following conversation has been lightly edited and condensed for clarity.
BIOPHARMA DIVE: Why did you license the treatment that became Kymriah to Novartis, rather than start a biotech around it?
CARL JUNE: That was a really big issue. We had offers from three large pharmas to in-license it to them, and then many offers to start a venture capital-based company. It was an ethical decision. Speed to market was important, because it was not a question of whether it would work, which it often is. By going to a pharma, there was no delay in building bricks and mortar and hiring people. They had a salesforce in place. We just had to teach their people to manufacture a cell therapy.
What did that experience teach you about working with a large organization?
JUNE: We had a mom-and-pop organization, and they had this army of people at Novartis. We had to learn how
to interact. We were much more nimble in making decisions, and that’s a real strength of biotech that I’ve now since realized.
The drawback of working with Big Pharma is large committees have to make decisions, rather than one person, like it used to be for us.
How did that impact your research?
JUNE: The license came in 2012, and then it became a high priority of ours to get this FDA approved in pediatric leukemia. And yet Kite [Pharma] — which was about two years behind us and had to put up the bricks and mortar and all that — caught up and was only [four] months behind us getting FDA approval. They played catch-up and really out-executed, as far as speed, what Novartis was able to do.
Did that influence your decisions since then to form biotech companies?
JUNE: Definitely. If you have a company that’s singularly focused, it can be more nimble, and that’s what I learned from the Kite versus Novartis experiments. Novartis has this huge portfolio and decision makers in Switzerland and Massachusetts. It just can’t keep up with a highly
focused team. That’s why I’ve gone now with Tmunity and Capstan. [Tmunity] has four [investigational new drug applications] that we’re filing this year. With Novartis, we couldn’t do that.
There have been setbacks as well for Tmunity. A clinical hold over safety. The company’s CEO left. Where do things stand?
JUNE: When you do Phase 1 trials, that’s when you really learn what the toxicities are. Then you have to either kill the program, figure out how to manage the toxicities, or go back and engineer a new kind of T cell.
That’s what Tmunity has done. Tmunity has opened their trial [back] up with a modified CAR design now … Our trials [at UPenn] opened up at a lower dose. We’re having efficacy, and manageable toxicity now. We’ll see. In 2023 hopefully enough data will be made to get dosing set for a registration trial. I think prostate cancer might be the first solid cancer where CAR-T cells get FDA approval.
How did Capstan come together?
JUNE: Sometime in 2018, John Epstein, a cardiologist and developmental biologist, told me about finding that
in injured hearts, these activated fibroblasts appeared that had fibroblast activation proteins. We had been building CARs against [those proteins], but for cancer. We started asking, ‘Can we target heart failure in mouse models?’ It was amazingly effective and published in Nature.
Then with Drew Weissman we started adapting [the process] to inject nanoparticles that can insert RNA into T cells in vivo and make CAR cells that can cause cardiac repair. That led to a paper in Science showing the feasibility of treating an animal model with in vivo CAR delivery.
Why form a new company around it?
JUNE: It’s a radically different manufacturing approach. What I have learned from Tmunity is, no biotech can really handle more than three or more projects at one time. Tmunity has four trials that are, or soon will be, open. There’s no way they could handle what we’re doing with Capstan. So that was an easy decision. It had to be a separate spin-out.
What makes in vivo CAR-T, particularly using mRNA, a challenge?
JUNE: Our immune system is primed to attack anything that’s delivering RNA. So the main challenge is, how do you make it stealth and get it into cells without causing a lot of immune activation? In the Science paper, we got 20% of the T cells in a mouse to express that CAR with a single injection. Will the profile be the same in humans as it is in mice, where we got very high levels of efficacy with very little toxicity?
What is your view of cell therapy’s potential for autoimmune disease?
JUNE: There was a Nature Medicine paper a couple of weeks ago where young women with refractory lupus, all between 20 and 24, had a response to CAR-T cells that were made almost identically to the way we made them to treat leukemia. We don’t yet know how long this will last or whether the toxicity is the same in patients with autoimmunity as they will be with cancer patients. It’s very early days, but it’s exciting for the field to see this possibility now. It could be a paradigm shift if cell therapies have a curative effect for any type of severe autoimmune disease.
What about allogeneic, or ‘off-the-shelf,’ cell therapy? It’s further along than autoimmune cell therapy, but there are questions about how effective it is.
JUNE: I actually think we’re going to have both. Autologous cells are more complex, but we know now that they persisted, in our initial patients, for 10 years, acting as a true living drug.
Allogeneic cells won’t do that, I don’t think, but they’re going to be much more readily available. They’ll be better able to be used in more rural areas.
Can allogeneic cells be made to persist longer and match the durability of CAR-T?
JUNE: If you made a cell so that you couldn’t reject it, which is what you would have to do to have an allogeneic cell persist like the autologous cells would, that’s actually a liability.
There is a whole class of viruses that can infect T cells. If you got an infection in one of these allogeneic cells that have been engineered so you can’t reject it, you would end up getting lymphoma. You actually don’t want them to last long term. You want them to last at most, a few weeks and then get rejected or just go away so that they’re not a liability long term. If the cells do persist long term, it’s just a matter of time until it will happen.
Are there similar problems with natural killer-based cell therapies?
JUNE: They have a great promise but they’re not designed to last long. NK cells last about a month — which is good. That’s actually a safety feature. They don’t cause graft-versus-host disease. They have an effect and then go away.
But in general, to have an actual clinical effect, they need to be a bridging therapy to a bone marrow transplant, other types of biologics, or even autologous cell therapy — to give you the time to make a precise engineered cell therapy. Because right now there’s been a lot of patients [for whom] that time just isn’t there. I think they’re actually mutually beneficial approaches and we’re going to see combinations of T cells and NK cells.
https://www.biopharmadive.com/news/carl-june-in-vivo-car-t-capstan-tmunity/633980/



ارسال به دوستان